VIDEO: Estes Park Health offers surgical repair for hernias
Stan Havlick of Estes Park is a self-described adventurer, speaker, and philanthropist. He has visited every continent around the globe in his 80 years. He’s an active retiree, but a recent pain in his abdomen sent him to the doctor for help.
“For a number of months, I had some discomfort in the lower abdomen,” Havlick explained. “I was talking to a doctor friend. He did a little probe and said, ‘You should have that looked at.’ It’s going to hamper my life and it’s uncomfortable a good part of the time, so I said, ‘Let’s just address this and get it out of the way.’”
Havlick had a hernia.

Estes Park Health general surgeon, Dr. Chris Bogardus, is a member of the American College of Surgeons, the American College of Osteopathic Surgeons, and the American Osteopathic Association. (Photo courtesy Dr. Chris Bogardus)
“An inguinal hernia is a defect in the abdominal wall that can allow either fat or muscle or even bowel to go through,” said Estes Park Health general surgeon Dr. Christine Bogardus. “It can cause pain. It can cause pressure and discomfort. Some people only see it. So, they get this little bulge in their groin that keeps getting bigger and bigger and bigger. Or some people only feel pain or pressure. They don’t see anything, but it is there. We can see it on CT scans, sometimes with ultrasound depending on the size, or on MRIs.”
Men are ten times more likely to develop this type of hernia which, if left uncorrected, can trap the bowel, and cause serious issues. That’s why Havlick opted for surgery at EPH.
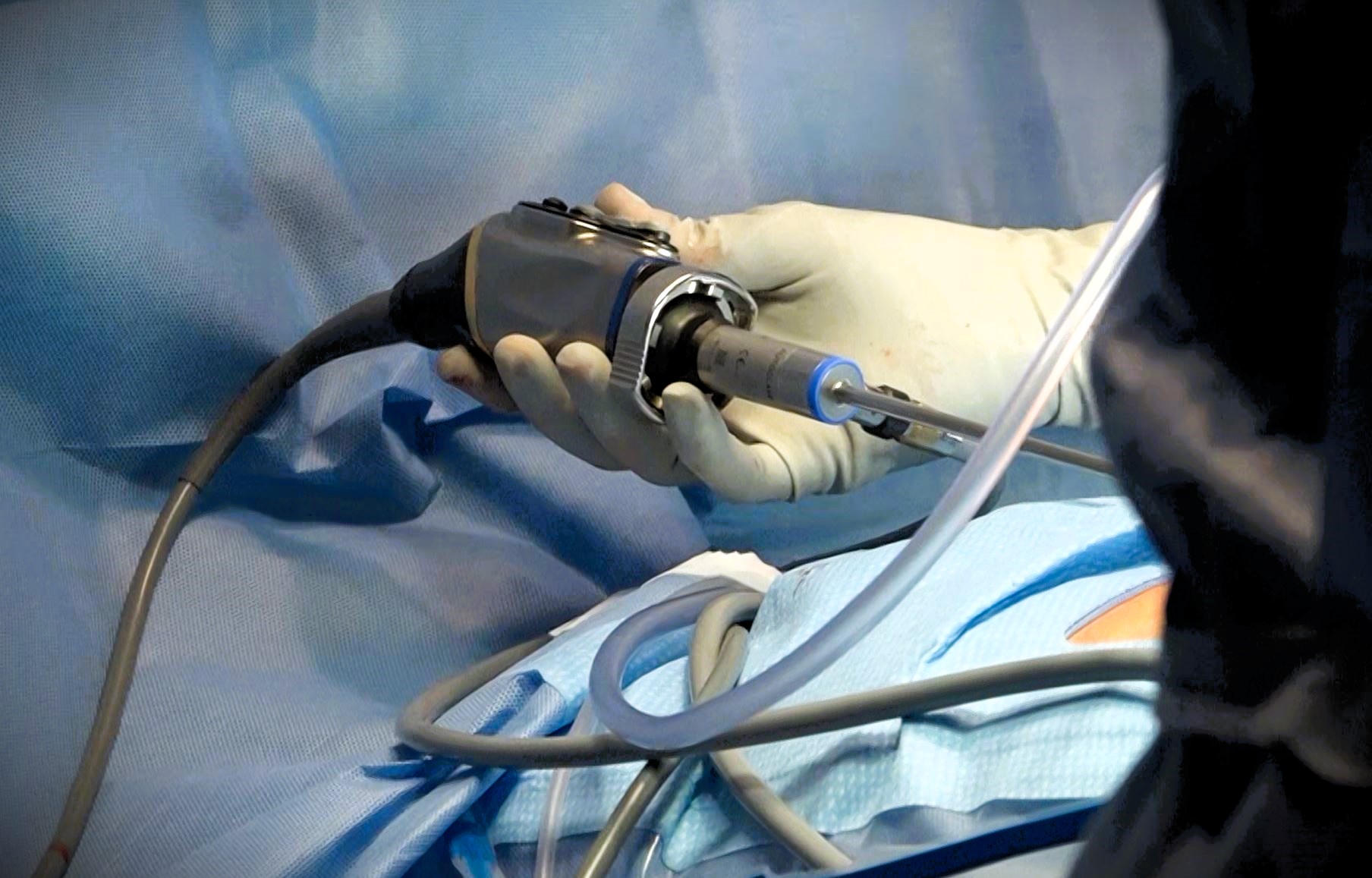
After Havlick was put under general anesthesia, Dr. Bogardus began the laparoscopic hernia repair. The procedure includes three small incisions. The largest one – about an inch – is at the belly button. An anesthetic block is placed underneath the muscle in the fascia to target the specific nerves that innervate the abdomen. In a one to two-hour procedure, Dr. Bogardus uses a lighted camera inserted through one of the holes to allow her to visualize what she is doing on a screen. The biggest challenge is getting her tools in the right place underneath the rectus muscle.
“I do a special procedure called a TEP — total extraperitoneal repair of the hernia — in which I don’t actually go into the belly at all,” Dr. Bogardus stated.
After the repair of the hernia, Dr. Bogardus placed a mesh, a composite of sheep gut and polypropylene, underneath the muscle and below the layer of the abdominal wall to strengthen the repair and reduce the risk of recurrence. Stan will not need any formal rehabilitation; however, the initial stages of recovery can be painful.
“I always tell my patients they’re going to feel like they got kicked by a cow for the first few days,” Dr. Bogardus stressed. “But after that, it tends to get better every day. A lot of people don’t even need narcotics anymore.”
Havlick went home the same day as his surgery.

Stan Havlick of Estes Park is prepped for hernia repair surgery. (Photo by Wendy Rigby/Estes Park Health)
“We highly recommend patients to go home because when they are home, they are comfortable,” Dr. Bogardus noted. “They tend to walk more when they’re not attached to things, which we strongly encourage.”
More than a million hernia repairs are performed by surgeons in the U.S. each year. It’s a highly effective way to get rid of a nagging and potentially dangerous problem.
Havlick was pleased with his experience at EPH, and happy to have his problem resolved. He will be back to enjoying his adventures.
“The whole crew was just terrific,” he added.
For expert general surgery care from highly trained community-based physicians, think Estes Park Health.


